News
Zero tolerance
Zero tolerance
The practice fully supports the NHS zero tolerance policy. The aim of this policy is to tackle the increasing problem of violence against staff working in the NHS and ensures that doctors and their staff have a right to care for others without fear of being attacked or abused.
We understand that ill patients do not always act in a reasonable manner and will take this into consideration when trying to deal with a misunderstanding or complaint. We ask you to treat your doctors and their staff courteously and act reasonably.
All incidents will be followed up and you will be sent a formal warning after a second incident or removed from the practice list after a third incident if your behaviour has been unreasonable.
However, aggressive behaviour, be it violent or verbal abusive, will not be tolerated and may result in you being removed from the practice list and, in extreme cases, the police will be contacted if an incident is taking place and the patient is posing a threat to staff or other patients.
Removal from the practice list
A good patient-doctor relationship, based on mutual respect and trust, is the cornerstone of good patient care. The removal of patients from our list is an exceptional and rare event and is a last resort in an impaired patient-practice relationship. When trust has irretrievably broken down, it is in the patient’s interest, just as much as that of the surgery, that they should find a new practice. An exception to this is on immediate removal on the grounds of violence e.g. when the police are involved.
Removing other members of the household
In rare cases, however, because of the possible need to visit patients at home it may be necessary to terminate responsibility for other members of the family or the entire household. The prospect of visiting patients where a relative who is no longer a patient of the practice by virtue of their unacceptable behaviour resides, or being regularly confronted by the removed patient, may make it too difficult for the practice to continue to look after the whole family. This is particularly likely where the patient has been removed because of violence or threatening behaviour and keeping the other family members could put doctors or their staff at risk.
Important Notice

Healthier Together
ADHD Medication prescribing in adults
Dear patients,
We have recently had to reject several new requests for ADHD medication prescribing in adults. This letter is aimed at explaining the reasons for it.
What should be happening?
The NHS ADHD service is commissioned to assess, diagnose, start medication, titrate medication and provide post-diagnostic reviews.
Once a patient is stable, the ADHD specialist enters a ‘shared care agreement’ (SCA) with the GP for ongoing prescribing to take place whilst still leading the care of the patient.
SCA is a carefully crafted, well-established and pre-arranged agreement with defined responsibilities for both specialist and GP
What is the problem?
National guidance expects long term involvement of specialists in reviewing ADHD patients and their medical treatment, but this does not currently happen in Oxfordshire. This then leaves GPs in a difficult position if we agreed to prescribe medications that we are not trained or funded to monitor. It is for this reason the practice has taken the decision not to accept any new requests from specialists, be it NHS or private, to prescribe ADHD medications to adult patients. This is in keeping with our Local Medical Committee’s recommendation.
Please be advised we will not be able to make any exceptions to this decision.
Care of adults already receiving ADHD treatments remains under careful review.
What then?
Patients may be able to access the care they need outside of the NHS, for instance by seeking a referral to a private provider.
Oxford Health that provides the NHS Adult ADHD service in Oxfordshire is not taking new referrals. The only NHS option for adult ADHD assessment is through the” right to choose” provision. Should you choose to go down either of these routes though, any prescriptions for medication will have to be provided by the specialist themselves.
We recognise the distress this might cause ADHD sufferers but sadly GPs cannot be expected to take on additional medico-legal risk because of a lack of NHS specialist provision. If you wish to raise this issue, then you may want to contact the “planned care team” at BOB ICB, bobicb.plannedcare@nhs.net , and/or your MP
Yours sincerely
Dr.T.Hurst
Dr.S.Ramani
Dr.C.Rose
Dr.K.Kommu
Dr.J.McGillvray
ADHD MEDICATION PRESCRIBING IN CHILDREN AND ADOLESCENTS
Child and adolescent NHS ADHD services in Oxfordshire are currently open to new referrals, but there are lengthy waiting lists to be seen. Where appropriate, we will consider sharing care with Oxfordshire CAMHS under a NHS shared care agreement,as long as they abide by the conditions set out in the agreed NHS shared care policy. When they are discharged from CAMHS aged 18 this shared care agreement comes to an end. At this point the named CAMHS consultant will be responsible for transferring their ongoing care, if still required, to adult services.
Due to the long NHS wait times a number of parents are seeking assessment for their children from private organisations. Unfortunately we are no longer able to enter into “shared care agreements” with private providers and therefore will be unable to prescribe any ADHD medication in this situation. This applies to Right to Choose providers as well and any referral made under the scheme will be for a diagnostic assessment only. The prescriptions of ADHD medications already being received by children remains under review.
Patients should not be left without the care they need, due to a lack of comprehensive NHS funding.Our local representatives have raised this issue with local funding and decision-making groups. If you also wish to raise this issue, you may want to contact the “planned care team” at the local Integrated Care Board, bobicb.plannedcare@nhs.net , and/or your MP
Drink coach

- Sharing your data with NHS Digital - FORM to OPT OUT
- doc06521720210607094233.pdf
Banburyshire Advice Centre support
Banburyshire Advice Centre supports many patients at other surgeries in the Banbury area who need help applying for Blue Badges, benefits and general advice working closely with Social Prescribers. We are also able to issue Food vouchers to those in need.
We are able to provide general advice and Career Advice. However, we cannot provide debt or legal or Tax advice but can refer or signpost onto other agencies.
The charity is very fortunate in that we can arrange free initial advice for Wills and Power of Attorney for our clients.
We are very happy to support your patients who may need our expertise. A referral is quick and easy.
You can send an email to this address: helpdeskbancp@yahoo.com with the outline of the problem or contact details and we can do the rest
or you can phone us up and leave a message on 01295 279988
Hearing Impairment Team
We are conscious that some patients registered at Bloxham and Hook Norton Surgeries may be affected by current events in Afghanistan. Bloxham and Hook Norton Surgeries are accredited by the Royal College of General Practitioners as one which specialises in the care of military veterans and their families. All the team have been trained in the care of military veterans and their families. If recent events have affected you and you wish to seek help, please come forward.
Age UK
Age UK Oxfordshire has launched a new scams prevention and support programme for older people in Oxfordshire area.
We are able to offer group talks to raise awareness of scams and also 1 to 1 sessions for those who have been affected by scams.
The programme, funded by Lloyds Banking Group, will help to prevent older people from falling for scams by increasing their knowledge and confidence to recognise and deal with attempted scams. It will also provide support to older fraud victims recovering after an incident.
Older people can be particularly vulnerable to fraud and scams, which can have a serious emotional and financial impact, and can damage quality of life and wellbeing for many.
Sophisticated scams have been on the rise during the pandemic with criminals devising even more ways to target those they believe to be vulnerable. This means it’s even more vital to support those that may be at greater risk.
We’re really pleased to be launching the Age UK Scams Prevention and Support Programme in the Oxfordshire area. Scams can have a devastating effect on older victims - in England and Wales an older person becomes a victim of fraud every 40 seconds, which is over 800,000 older people every year. This shows us just how important this programme is to try and keep the older people in Oxfordshire as safe as possible when it comes to financial crime.
Contact Us
To find out more about Age UK Oxfordshire’s Scams Prevention and Support Programme, please contact: 0345 450 1276.
The GP Practices and Health Centres of the North Oxfordshire Rural Alliance Primary Care Network partners with some third parties to provide specific healthcare and social prescribing services. These third parties are signed up to Data Sharing Contracts with the North Oxfordshire Rural Alliance and the information they are supplied with is limited only to that of the patients that they have appointments with. The third party companies do not retain, share, store or use personally identifiable information for any secondary purposes.
If you would like further information on the third parties we work with, please contact the Practice Manager
Visiting the UK? You may be chargeable for NHS Treatment

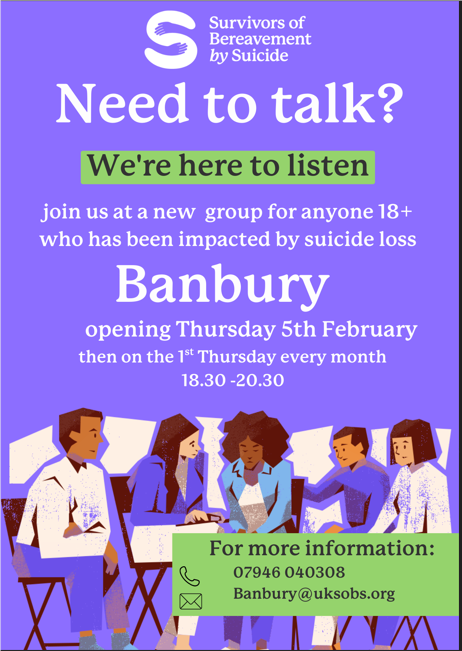
SOBS Group
Page created: 01 October 2020